
AI-generated patient-specific finger joint implant
Current research



Patient-specific joint implants promise a better fit and thus improved functionality and a longer service life than conventional implants. Especially for small joints, where the possibilities for remobilization are currently limited and stiffening is the standard therapy, individual implants offer better care options and an increase in the patient‘s quality of life.
As part of the project “FingerKit”, the Fraunhofer institutes IKTS, MEVIS, IAPT, ITEM and IWM have developed an autonomous process chain from implant design to the production of patient-specific implants and standard-compliant testing.
Shape model, implant design and simulations
On the basis of clinical 2D X-ray data and 3D CT images, Fraunhofer MEVIS generated 3D shape models of the bone structure. Building on this, Fraunhofer IAPT was able to generate an AI-based patient-specific implant design. Fraunhofer IWM created a model predicting the design’s reliability using parameterization and simulation.
Near-net shape slip casting for patient-specific finger joint implants
Ceramics have excellent mechanical properties in addition to high wear resistance and biocompatibility. They are considered to be more tolerable than metallic and plastic implants, which have a high occurrence of abrasion. In hip endoprosthetics, dispersion ceramics, such as alumina-reinforced zirconia (ATZ), have become particularly well established.
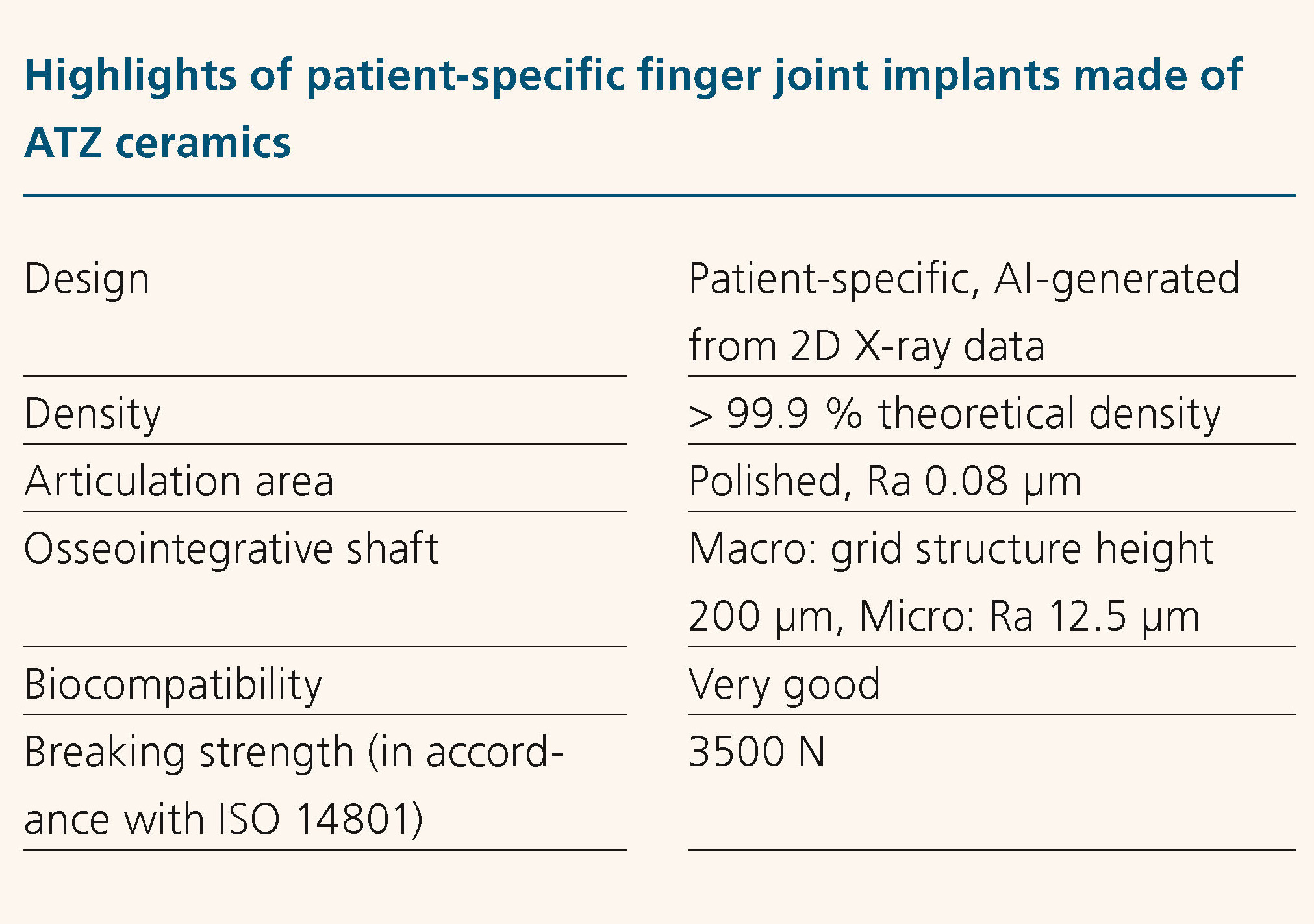
At Fraunhofer IKTS, patient-specific finger joint implants made of the established oxide ceramic implant material ATZ were manufactured in a single step using slip casting. In contrast to conventional production by milling, the osseointegrative surface of the stem does not require any additional finishing. The process achieved a cross structure with a height of 200 µm, the surface of which has a roughness of Ra 12.5 µm, ensuring ideal cell adhesion.
Thanks to an easy-to-scale vibratory grinding and polishing procedure, the articulatory and contact surfaces were of high quality and very robust, and material abrasion was prevented. The implants’ mechanical load capacity of up to 3500 N exceeds many times over the 500 N loads occurring in vivo in the implanted state.
The process chain from AI-based generation of the implant design to near-net shaping of ATZ shows great potential for extending the approach for patient-specific implants to other small joints.